CARDS FROM 2 TO 7 OF CUPS
ASTROGLIA IN NEURODEGENERATIVE DISEASES
Cards from 2 to 7 of cups: astroglia in neurodegenerative diseases
Our suit of Cups is represented by astrocytes, glial cells that provide such a complete menu of services to neurons that, when any ingredient is missing from the dishes on the menu, problems arise associated with many neurological diseases.
There are more than 600 diseases of the nervous system of a multiple and diverse nature, which neuroscientists investigate to, knowing their causes, design their possible treatments.
Among the neurological diseases we can mention behavioral diseases and dementias (such as Alzheimer’s or dementia with Lewy bodies); demyelinating diseases (such as multiple sclerosis); neuromuscular diseases (there are 150, including ataxias and movement disorders such as Parkinson’s disease or Huntington’s disease); infections of the nervous system (such as spongiform encephalopathies caused by prions); epilepsy; vascular diseases (such as strokes); migraine and other headaches; brain tumors (such as gliomas); traumatic conditions of the nervous system; development disorders of the nervous system, or toxic-metabolic and deficiency disorders, without forgetting sleep disorders and other disorders such as those on the autism spectrum [1][2].

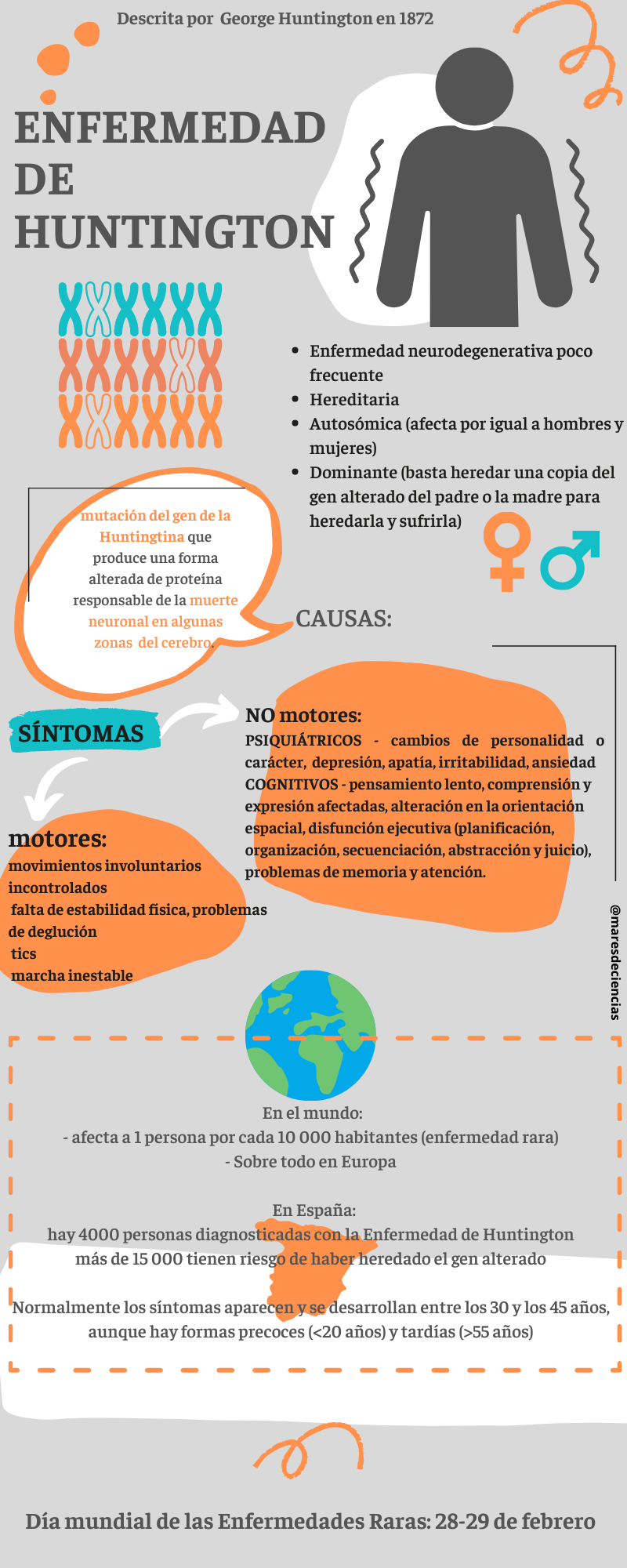
It is known that some are hereditary (such as Huntington’s disease, peripheral neuropathies such as Charcot-Marie-Tooth disease, ataxias such as Friedreich’s or dystrophies such as Duchenne and Becker) and for one of them, Huntington’s disease, The mutant gene that causes it has been located in the human genome. This allows the disease to be identified before its symptoms appear, to anticipate its consequences and refine treatments. Other diseases, such as multiple sclerosis, are of autoimmune origin, although it is unknown what causes the individual’s immune system to attack its own nervous structures. The exact causes of many neurological diseases are unknown, but it is very likely that there is genetic susceptibility and risk factors (hereditary or not) that increase the chances of suffering from them, although they are neither sufficient nor necessary to suffer from them.
Within the range of diseases of the nervous system, neurodegenerative diseases are the most prevalent today, since they are closely related to the generalized aging of the population, which is increasingly numerous and has a longer life expectancy. When in previous posts we talked about Alzheimer’s disease and multiple sclerosis, we saw that they all tend to evolve progressively, in addition to affecting not only the person who suffers from them but also their closest environment [1]. For this reason, the World Health Organization has warned that they have become a global health problem with serious consequences, both human, social and economic, that must be addressed urgently.
Neurodegenerative diseases are chronic processes that are characterized by the progressive death of neurons in different regions of the nervous system, which causes functional deterioration of the affected parts, whether motor, sensory or cognitive. This gradual loss of nerve cells is responsible for the neurological and neuropsychological signs and symptoms that characterize them [3].
Although in our neurodeck we associate Alzheimer’s disease with neurons (because, among other things, axon deterioration occurs), and multiple sclerosis with oligodendrocytes (as it is a demyelinating disease), the truth is that it is impossible to attribute a single type of nerve cells responsible for neurological diseases. What is certain is that astrocytes intervene in some way in most of them. Can you guess why?
Well, because astrocytes are the most abundant glial cells in the central nervous system and because they are essential for its proper functioning. Not only do they participate in forming the framework that structures and physically supports the nervous tissue, but they also protect the brain from the entry of pathogens (thanks to the blood-brain barrier); They intervene in metabolic regulation and in the recycling of neurotransmitters; they manage the glycogen reserve (to supply the necessary energy at the demand of the neurons); They control and regulate blood flow that provides oxygen and nutrients to neurons; They modulate neuronal activity and intervene in the way nervous information is processed; They participate in tripartite synapses and assume functions related to neuronal development and plasticity. In addition, astrocytes coordinate the production of myelin and collaborate with microglia in defensive tasks. Therefore, it is logical that the malfunction of astrocytes is involved in neurological diseases, especially neurodegenerative diseases, and is even closely related to neuropsychiatric symptoms [13].
The most recent studies provide physiological and pathological evidence of the range of forms and functions of astrocytes, which constitute a varied population of cells with very specific functions dependent on the neural circuits in which they intervene as modulators [4]. Thus, in the human brain, together with the protoplasmic astrocytes of the gray matter that participate in tripartite synapses and the fibrous astrocytes associated with neuronal axons in the white matter, there seems to be a third type of reactive astrocytes. Although there are no prototypical reactive astrocytes, because we have already said that they adopt different states depending on the context in which they are found, faced with any damage or threat (vascular accident, disease or infection) they react with morphological, molecular and functional changes [6] that They can be neuroprotective or, on the contrary, harmful depending on the pathological context and the nervous circuits or microcircuits in which they are involved. This activation is heterogeneous and variable: when it is neurotoxic it seems to involve the M1 phenotypes of microglia and A1 of astrocytes, and when it is neuroprotective it is the M2 phenotypes in microglia and A2 in astrocytes [5].
An example of this occurs when astrocytes assume defensive functions together with microglia to deal with certain brain injuries by forming the so-called glial scar, or by participating in the physiological processes of neuroinflammation triggered to combat any disturbance in the nervous tissue.
The glial scar forms in the event of severe injuries and is essential in the repair of damaged tissue of the central nervous system, as it functions as a cell migration barrier around areas where intense inflammation is needed, restricting the spread of inflammatory cells and agents that damage adjacent healthy tissue [15].
Neuroinflammation is closely associated with neurodegenerative diseases such as Alzheimer’s, Parkinson’s, or amyotrophic lateral sclerosis (ALS) and at the heart of this response are the morphological, molecular and functional changes of both microglia and astrocytes.
It seems clear that abnormalities in astrocytic function are related to the onset of many neurodegenerative diseases [9]. Thus, the role that changes in astrocyte function play in diseases of the central nervous system may be due to [5][7][8][4]:
to the negative effects derived from the loss of neuroprotective functions of astrocytes (partial, because some studies [2] suggest that even in pathological situations all or part of the astrocytes maintain them);
to excess astrocyte reactivity that can be toxic, or
to a combination of both.
The response of astrocytes to any type of damage, injury or infection is carried out through a process called “astrogliosis” [14]. Let’s see broadly what role astrocytes play in some of the main neurodegenerative diseases.
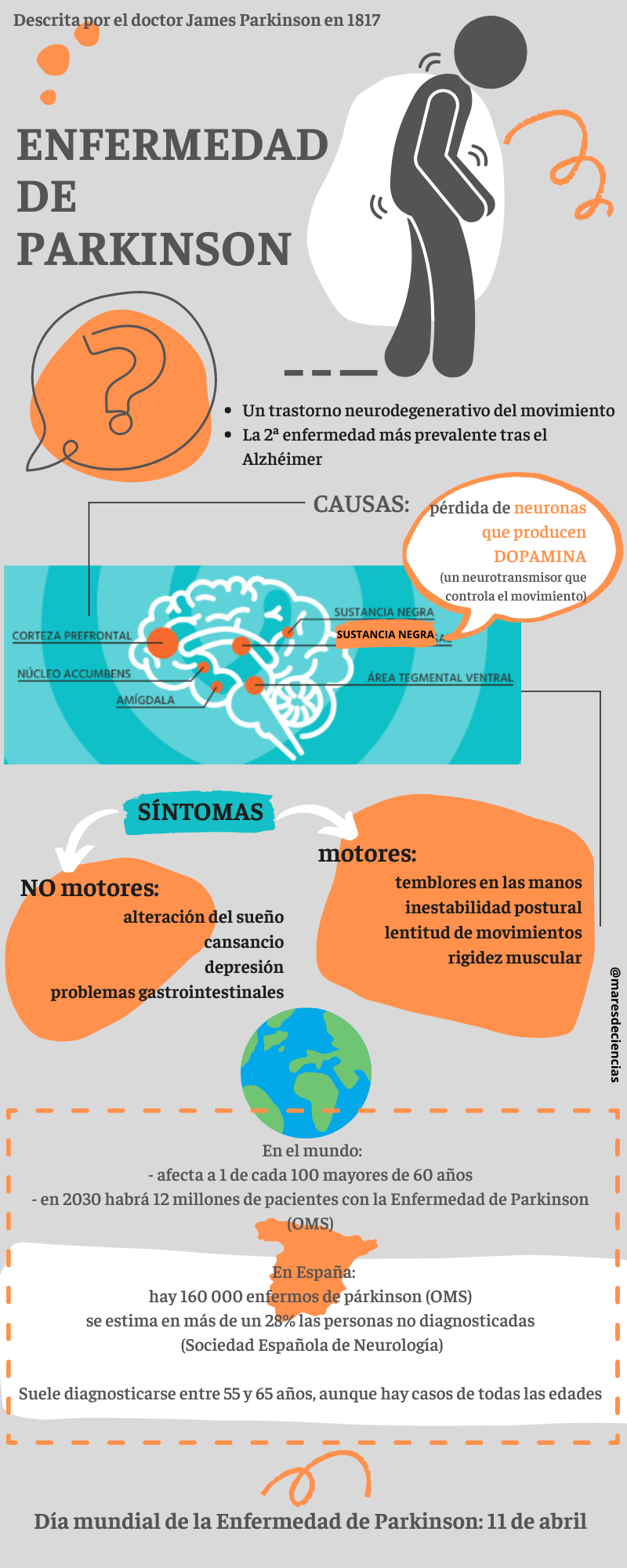
– In Parkinson’s disease, intraneuronal aggregates of α-synuclein, called Lewy Bodies, are formed. It appears that α-synuclein can also accumulate in the cytoplasm of protoplasmic astrocytes, leading to the activation of microglia and the production of neuroinflammatory mediators. Problems with the regulation of the blood-brain barrier and with the metabolism of glutamate, whose accumulation is toxic to neurons, have also been observed [8].
– In Huntington’s disease, the mutation in the HTT gene produces a mutant protein (called huntingtin) that not only damages neurons. In astrocytes, this disease causes alterations in calcium signaling, problems with the recycling of neurotransmitters (such as glutamate) and the regulation of potassium concentration, as well as dysfunctions in mitochondria, excess cholesterol and the acquisition of a phenotype reagent related to neuroinflammation [8][14].
– In amyotrophic lateral sclerosis (ALS) astrocytes stop correctly recycling glutamate, which accumulates in the extracellular environment. Dysfunctions also appear in lactate transport and with reactive oxygen species, so that everything contributes to creating toxic factors that activate the microglia pathway and cause damage to motor neurons. Astrocyte-neuron reciprocal communication also seems to be altered, so that together a series of very complex multicellular interactions occur that, among other things, activate programmed cell death mechanisms (apoptosis) [8].
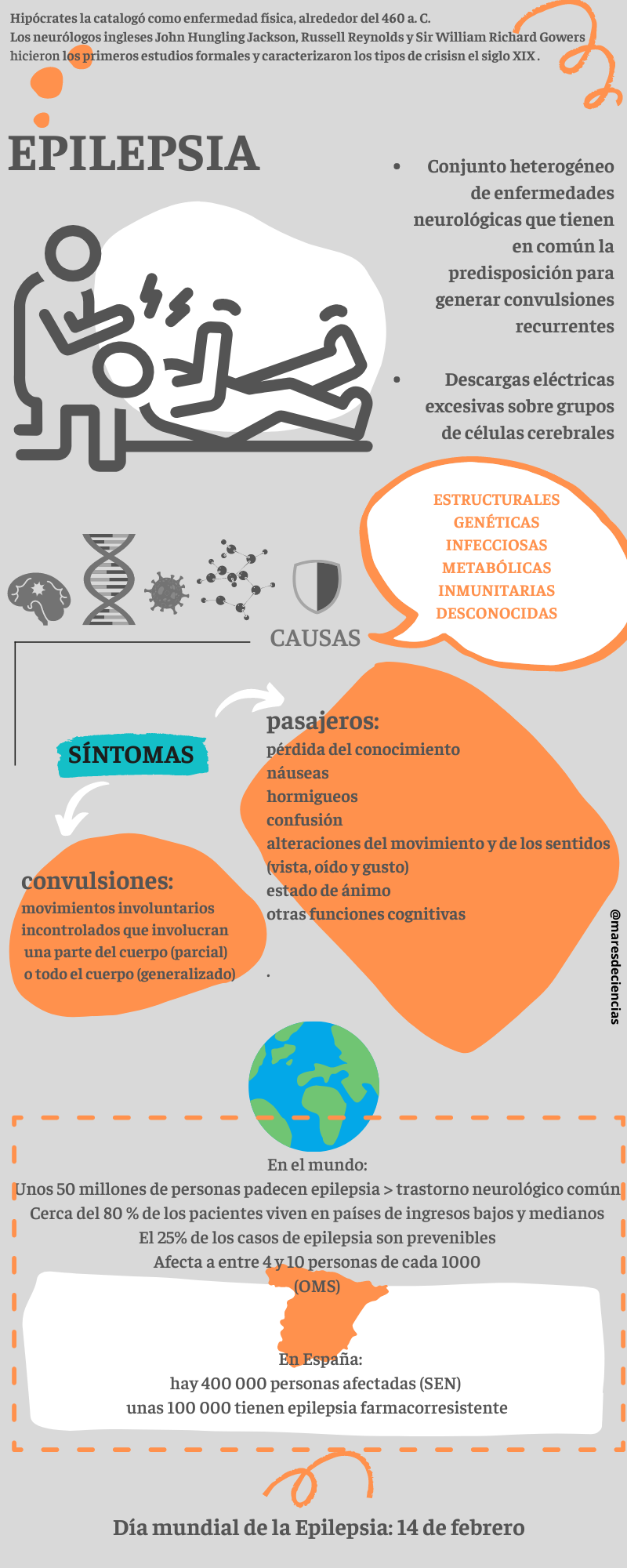
– In epilepsy it seems that astrocytes are involved in the seizure synchronization mechanism. Again, inactivation of glutamate transporters appears to occur, favoring excitatory synapses and disturbing homeostasis [8].
– In Alzheimer’s disease, it is the β-amyloid plaques that impact the poor functioning of astrocytes: calcium homeostasis, energy and oxidative metabolism are altered, so that astrocytes become toxic to neurons [8].
What is clear is that there are very complicated relationships between these reactive glial cells and there are still many unknowns to be resolved in the phenomena of astrocyte plasticity that allows them to promote inflammation (pro-inflammatory phenotypes) or fight against it (anti-inflammatory phenotypes) [ 6]. In this sense, lines of research are currently directed both at identifying biomarkers of neuroinflammation and therapeutic targets that can help test drugs capable of modulating it, and at unraveling the mechanisms behind astrocyte plasticity to exploit them for therapeutic purposes [7 ] [eleven]. There are even plans to exploit this plasticity and the numerical abundance of astrocytes to convert them into neurons to replace those destroyed by the disease [12]. Surprising, right?
Have you been curious and want to know more?
Patient associations:
SPANISH PARKINSON FEDERATION https://www.esparkinson.es/la-federacion/
SPANISH ASSOCIATION OF AMYOTRIPHIC LATERAL SCLEROSIS (adELA) https://adelaweb.org/
SPANISH KOREA HUNTINGTON ASSOCIATION (AECH) https://www.e-huntington.es/
NATIONAL ASSOCIATION OF PEOPLE WITH EPILEPSY (ANPE) https://www.anpeepilepsia.org/
NOTES AND SOURCES CITED:
[1] GARCÉS, Mario (2016). Study on neurodegenerative diseases in Spain and their economic and social impact. Documentary report prepared by “Neuroalianza” (Spanish Association of Neurodegenerative Diseases) and the Complutense University of Madrid, 180 pp. https://eprints.ucm.es/id/eprint/43893/1/Informe%20NeuroAlianza%20Completo%20v.51.pdf
[2] ZHOU, Y., SHAO, A., YAO, Y., TU, S., DENG, Y., and ZHANG, J. (2020). Dual roles of astrocytes in plasticity and reconstruction after traumatic brain injury. Cell Commun. Signal. 18 (1), 62. doi:10.1186/s12964-020-00549-2
[3] DOMÍNGUEZ MONEDERO, A. and F. GOÑI DE CERIO (2014). Neurological diseases and their treatment. Pending challenges in pharmacology. Pharmatec Magazine, Special Biotechnology 2014 (10): pp. 40-44 https://www.pharmatech.es/descargar_documento/GAIKER.pdf
[4] DI CESARE MANNELLI, Lorenzo, Stefania CERUTI and Juan A. ORELLANA (2021). Publisher: Astrocytes, a Kaleidoscope of Diversities, a Pharmacological Horizon. Front Pharmacol 2021; 12: 638239. Published online March 8 doi: 10.3389/fphar.2021.638239
[5] GUILLAMÓN-VIVANCOS, T., U. GÓMEZ-PINEDO and J. MATÍAS-GUIU (2015). Astrocytes in neurodegenerative diseases (I): function and molecular characterization. Neurology (2015) 30(2): 119-129 https://www.elsevier.es/en-revista-neurologia-295-articulo-astrocitos-enfermedades-neurodegenerativas-i-funcion-S0213485313000042
[6] Reactive astrocytes: an unexplored therapeutic niche for neurological diseases. Research and Science, March 5, 2021 https://www.investigacionyciencia.es/blogs/psicologia-y-neurociencia/37/posts/astrocitos-retrabajos-un-inexplorado-nicho-teraputico-para-las-enfermedades-neurolgicas -19622
[7] KWON Hyuk-Sung and Seong-Ho KOH (2020). Neuroinflammation in neurodegenerative disorders: the roles of microglia and astrocytes. Translational Neurodegeneration (2020) 9:42 https://translationalneurodegeneration.biomedcentral.com/articles/10.1186/s40035-020-00221-2
[8] PHATNANI, H. and Tom MANIATIS (2015). Astrocytes in Neurodegenerative Disesase. Cold Spring Harb Perspect Biol 2015;7:a020628 DOI: 10.1101/cshperspect.a020628
[9] TRUJILLO-ESTRADA, L., A. GOMEZ-ARBOLEDAS, S. FORNER, AC MARTINI, A. GUTIERREZ, AND D. BAGLIETTO-VARGAS, FM La FERLA. Astrocytes: From the Physiology to the Disease. Curr Alzheimer Res. 2019;16(8):675-698. http://www.eurekaselect.com/article/100542
[10] Parkinson’s Disease is the second neurodegenerative disease, with the highest prevalence in our country. It affects more than 6.3 million people worldwide[1]
[11] GIOVANNONI, Federico and Francisco J. QUINTANA (2020). The Role of Astrocytes in CNS Inflammation. Trends in Immunology, Volume 41, Issue 9, 805 – 819 https://doi.org/10.1016/j.it.2020.07.007
[12] QUIAN, H., KANG X, HIAN, H., KANKG, X., HU, J. (2020). Reversing a model of Parkinson’s disease with in situ converted nigral neurons. Nature 582: pp. 550 to 556. https://doi.org/10.1038/s41586-020-2388-4
[13] BEN HAIM, Lucile and Carole ESCARTIN. Astrocytes and neuropsychiatric symptoms in neurodegenerative diseases: Exploring the missing links. Current Opinion in Neurobiology, Volume 72, 2022, Pages 63-71. https://doi.org/10.1016/j.conb.2021.09.002
[14] KHAKH, B. S., BEAUMONTt, V., CACHOPE, R., MUNOZ-SANJUAN, I., GOLDMAN, S. A., & GRANTYN, R. (2017). Unraveling and Exploiting Astrocyte Dysfunction in Huntington’s Disease. Trends in neurosciences, 40 (7), 422–437. https://doi.org/10.1016/j.tins.2017.05.002
[15] MARTÍNEZ TAPIA, R. J., F. ESTRADA-ROJO, A.A. HERNÁNDEZ-CHÁVEZ, A. BARAJAS-MARTÍNEZ, S. ISLAS ESCOTO, L. NAVARRO, A. CHAVARRÍA (2018). Neuroinflammation: The Ying-Yang of Neuroimmunology. Journal of the Faculty of Medicine (Mexico), 61 (5): 44-53
OTHER LINKS OF INTEREST
YouTube Channel Cerebrotes, by Clara García:
The importance of Huntington’s disease https://www.youtube.com/watch?v=QaHbf40DTuk
Intellectual activity and Huntington’s disease https://www.youtube.com/watch?v=oVlS13Pldso&t=192s
EMP Synapse YouTube Channel:
What is Parkinson’s? https://www.youtube.com/watch?v=39QtyibhWlM
What is epilepsy and seizures? https://www.youtube.com/watch?v=vzqJh–l1cs
SEGOVIA DE ARANA, José Mª and Francisco MORA TERUEL (coord.) (2002). Neurodegenerative diseases. Farmaindustria, Scientific Series Madrid, 2002 http://envejecimiento.csic.es/documentos/documentos/segovia-neurodegenerativas-01.pdf
Francesc Palau Martínez, Ana Cuesta Peredo, Javier García Planells, Pilar González Cabo, Laia Pedrola Vidal, Reyes Calaramunt Alonso and Carmen Espídos Armero (2004). HEREDITARY NEUROLOGICAL DISEASES: Genes, mutations, clinic and genetic epidemiology. Genetics and Molecular Medicine Unit, Institute of Biomedicine of Valencia (CSIC). Document 67/2005 “Memory of the research work awarded with the allocation for Spain of the 2004 Reina Sofía Awards, for Prevention of Deficiencies.” Royal Board of Trustees on Disability
Ashley M. INGIOSI, Christopher R. HAYWORTH, Daniel O. HARVEY, Michael J. REMPE, Jonathan P. WISOR and Marcos G. Frank. A Role for Astroglial Calcium in Mammalian Sleep and Sleep Regulation. Current Biology (2020). DOI: https://doi.org/10.1016/j.cub.2020.08.052 https://doi.org/10.1016/j.it.2020.07.007
CHNEIWEISS, H. (2005). Et l’épilepsie devint une maladie de l’astrocyte. MS / Médecine Sciences, Volume 21, number 12, December 2005, p. 1023–1025 https://www.erudit.org/fr/revues/ms/2005-v21-n11-ms1023/012003ar/
